Management of Specific Clinical Scenarios
Clinical Outline
= Primers in Thyroidology
= Journal Club Presentation
= Case-based Discussion (inc. roundtables)
= Grand Rounds Lectureship
Management Recommendations
1. Management of Inherited Forms
A. Prophylactic Thyroidectomy in Children with Inherited Forms of MTC including MEN2A & MEN2B
ATA // ESMO // NCCN
Experienced physicians and surgeons in tertiary care centers should be responsible for the management of children with MEN2A or MEN2B, in consultation with clinical geneticist.1,2
The surgeon and pediatrician caring for the patient, in consultation with the child’s parents, should decide the timing of thyroidectomy.1
Need paragraph here to explain categories and as a prelude to the table.
Tables & Figures
Table 12. Most Common RET Mutations with Associated Risks
RET Mutation
Highest Risk Level (HST)
M918T
| RET Exon | 16 |
| Risk of Aggressive MTC | Highest |
| Incidence of Pheochromocytoma | 50% |
| Incidence of Hyperparathyroidism | – |
High Risk Level (H)
C634F/G/R/S/W/Y
| RET Exon | 11 |
| Risk of Aggressive MTC | High |
| Incidence of Pheochromocytoma | 50% |
| Incidence of Hyperparathyroidism | 20–30% |
A883F
| RET Exon | 15 |
| Risk of Aggressive MTC | High |
| Incidence of Pheochromocytoma | 50% |
| Incidence of Hyperparathyroidism | – |
Moderate Risk Level (MOD)
G533C
| RET Exon | 8 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10% |
| Incidence of Hyperparathyroidism | – |
C609F/G/R/S/Y
| RET Exon | 10 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10–30% |
| Incidence of Hyperparathyroidism | 10% |
C611F/G/S/Y/W
| RET Exon | 10 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10–30% |
| Incidence of Hyperparathyroidism | 10% |
C618F/R/S
| RET Exon | 10 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10–30% |
| Incidence of Hyperparathyroidism | 10% |
C620F/R/S
| RET Exon | 10 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10–30% |
| Incidence of Hyperparathyroidism | 10% |
C630R/Y
| RET Exon | 11 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10–30% |
| Incidence of Hyperparathyroidism | 10% |
D631Y
| RET Exon | 11 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 50% |
| Incidence of Hyperparathyroidism | – |
K666E
| RET Exon | 11 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10% |
| Incidence of Hyperparathyroidism | – |
E768D
| RET Exon | 13 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | – |
| Incidence of Hyperparathyroidism | – |
L790F
| RET Exon | 13 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10% |
| Incidence of Hyperparathyroidism | – |
V804L/M
| RET Exon | 14 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10% |
| Incidence of Hyperparathyroidism | 10% |
S891A
| RET Exon | 15 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | 10% |
| Incidence of Hyperparathyroidism | 10% |
R912P
| RET Exon | 16 |
| Risk of Aggressive MTC | Moderate |
| Incidence of Pheochromocytoma | – |
| Incidence of Hyperparathyroidism | – |
Table adapted from Table 4, Wells et al, Revised ATA guidelines for the management of medullary thyroid carcinoma, Thyroid 2015. The publisher for this copyrighted material is Mary Ann Liebert, Inc. publishers.
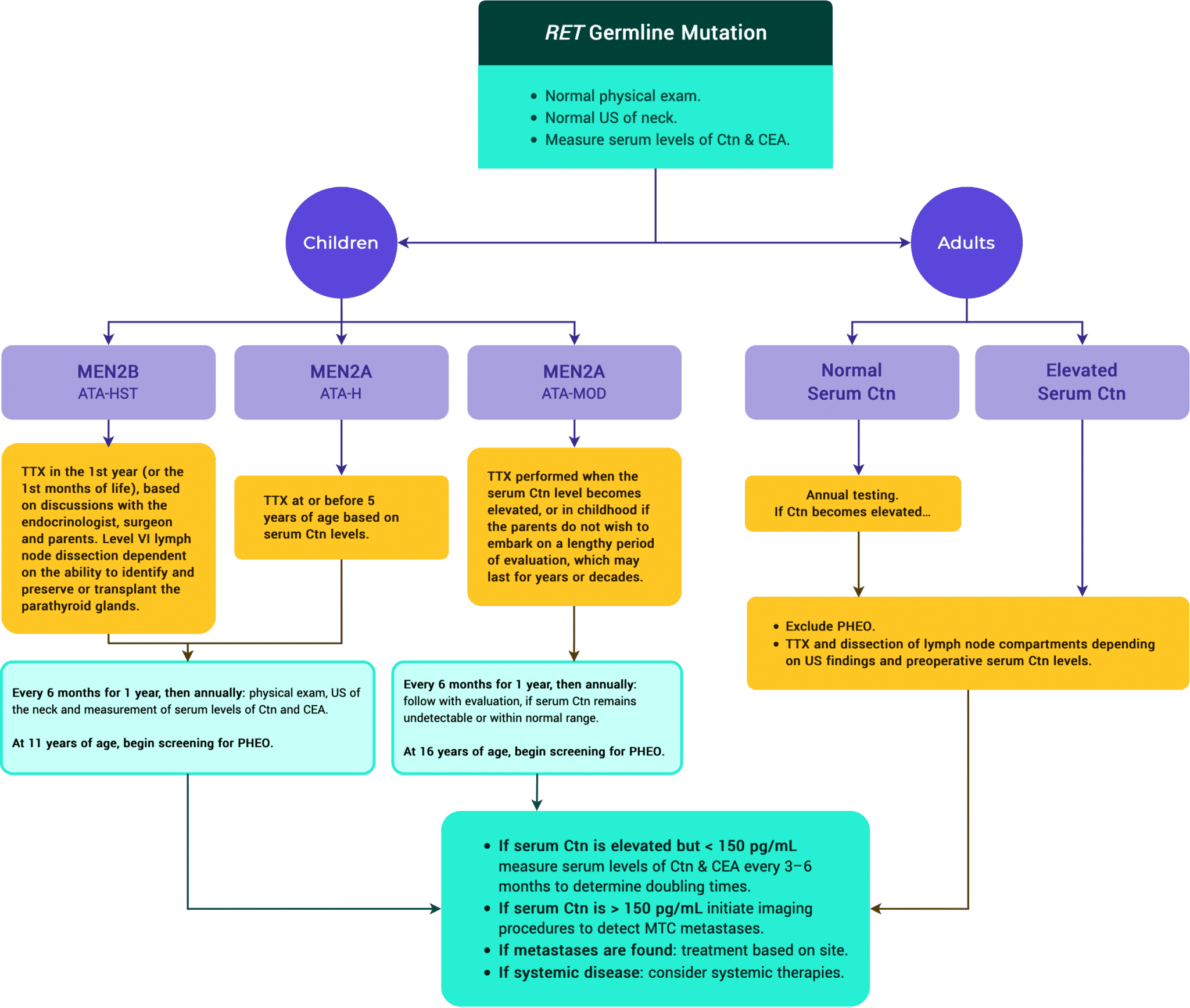
Children in the ATA-highest risk (HST) category with a RET codon M918T mutation should have a total thyroidectomy in the first year of life, perhaps even in the first months of life.1–3
Therapeutic neck dissection as indicated; consider prophylactic bilateral central neck dissection.2
Children in the ATA-high risk (H) category should have a total thyroidectomy performed at age 5 years, or earlier based on the detection of elevated serum Ctn levels.1–3
A central neck dissection should be performed in children with serum Ctn levels above 40 pg/mL, or with evidence on imaging or direct observation of lymph node metastases.1,2
Children in the ATA-moderate risk (MOD) category should have a physical examination, US of the neck, and measurement of serum Ctn levels beginning around 5 years of age.1,3
Prophylactic thyroidectomy may be delayed, provided the annual basal Ctn measurement is normal, the annual US is unremarkable, there is no history of aggressive MTC in the family, and the family is in agreement.1,2
While 6-month or annual evaluations may extend to several years or decades, parents who are concerned about a long-term evaluation program may opt to have their child’s thyroid gland removed around 5 years of age.1
The performance of a central neck dissection should be based on whether the parathyroid glands can be identified and left in situ or auto transplanted.1
Prophylactic Total Thyroidectomy
JAES
- Prophylactic total thyroidectomy is not uniformly recommended for asymptomatic carriers of RET mutations in Japanese guidelines.
Tables & Figures
Figure 12. ATA Management of Patients with RET Germline Mutation Detected on Genetic Screening.
B. Management of PHEO in Patients with MEN2A & MEN2B
ATA // ESMO // JAES // NCCN
PHEO screening should be done for patients with MTC. Evidence of PHEO should be evaluated and addressed appropriately before proceeding to the next step on the pathway. If they coexist, a PHEO should be removed prior to surgery for either MTC or HPT.1–4
Screening for PHEO and HPT should be performed annually. For the ATA-MOD category, less frequent screening may be appropriate. Screening for PHEO should begin by age 11 years for children in the ATA-H and ATA-HST categories and by age 16 years in children in the ATA-MOD category.1,2
Screening consists of measuring free plasma metanephrines and normetanephrines or 24-hour urinary metanephrines and normetanephrines. Adrenal imaging with CT or MRI is indicated in patients with positive biochemical results.1
Patients with MEN2A or MEN2B and a histological diagnosis of MTC regardless of age and presenting symptoms must have a PHEO excluded prior to any interventional procedure. The presence of a PHEO must be excluded in women with MEN2A or MEN2B who are planning a pregnancy or are pregnant. If a PHEO is detected it should be treated preferably prior to the third trimester.1
A PHEO should be resected after appropriate preoperative preparation. Laparoscopic or retroperitoneoscopic adrenalectomy is preferable. Subtotal adrenalectomy to preserve adrenal cortical function should be considered as an alternative procedure.1
Patients with no adrenal glands require glucocorticoid and mineralocorticoid replacement therapy and should be carefully monitored to ensure that their steroid levels are adequate. Patients should be educated regarding the risk of adrenal crisis and wear a bracelet or a necklace indicating that they have no adrenal glands and are on corticosteroid replacement therapy. Glucocorticoid supplementation will be required if they become severely ill or are injured.1
C. Management of HPT in Patients with MEN2A
ATA // NCCN
Patients in the ATA-H and ATA-MOD categories should be screened for HPT at the time of screening for PHEO (by age 11 years in patients in the ATA-H category and by age 16 years in patients in the ATA-MOD category).1
In addition to US, parathyroid imaging including sestamibi scan with SPECT or 4D-CT is recommended to determine surgical indication.2
In patients with HPT only visibly enlarged parathyroid glands should be resected. If all four glands are enlarged surgical options include subtotal parathyroidectomy with a piece of one gland left in situ on a vascular pedicle or total parathyroidectomy with a heterotopic autograft.ATA Cryopreservation of parathyroid tissue should be considered.2
Patients who develop HPT after thyroidectomy for MTC should have localization studies performed prior to repeat neck surgery. At reoperation all enlarged parathyroid glands should be removed, and parathyroids of normal size should be left in situ. If only one enlarged parathyroid gland is identified and there is histological documentation that three parathyroid glands have been removed previously, a portion of the enlarged gland should either be left in situ with an adequate blood supply or grafted to a heterotopic site.1
2. Management of Patients with Hormonally Active Metastases
Diarrhea is common in patients with advanced MTC and elevated calcitonin levels. This diarrhea can detrimentally affect quality of life and a patient’s nutritional status; therefore, treatment of the diarrhea is important. Patients with diarrhea should avoid alcohol and should be treated with antimotility drugs such as loperamide, diphenoxylate/ atropine, or codeine. Rarely, somatostatin analogs can be helpful.
Rarely the cancer cells produce ectopic corticotropin releasing hormone (CRH) or ACTH. This excessive hormonal production results in Cushing’s syndrome and elevated cortisol levels. Resulting symptomatic diabetes, weakness, hypokalemia, hypertension, and gastritis in patients with ectopic Cushing’s syndrome should be evaluated for and treated. Given that this syndrome is debilitating, Cushing’s syndrome should be treated despite the poorer overall survival. For control of cortisol levels and these symptoms, one can initiate anti-cortisol therapies such as ketoconazole, mifepristone, aminoglutethimide, metyrapone, or mitotane. Bilateral adrenalectomy should also be strongly considered.
Treatment of the underlying metastatic medullary thyroid cancer with systemic therapies, metastatectomies, debulking surgeries, radiation, or ablation of various metastases (especially hepatic metastases) can aid with relief of these hormonally active metastases, namely, diarrhea & ectopic Cushing’s.1

Add Upcoming TIROxMDS Seminars to Your Calendar
In 2 quick steps, you can add our entire schedule of upcoming seminars to your calendar today! Then you will get notified of upcoming lectures, presentations and case-based studies. Every Friday at 8:00 AM EST, we cover a new topic from published research.
Add to CalendarReferences
- 1.Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. Published online January 2016:1-133. doi:10.1089/thy.2015.0020
- 2.Haddad RI, Nasr C, Bischoff L, et al. NCCN Guidelines Insights: Thyroid Carcinoma, Version 2.2018. J Natl Compr Canc Netw. Published online December 2018:1429-1440. doi:10.6004/jnccn.2018.0089
- 3.Filetti S, Durante C, Hartl D, et al. Thyroid cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology. Published online December 2019:1856-1883. doi:10.1093/annonc/mdz400
- 4.Ito Y, Onoda N, Okamoto T. The revised clinical practice guidelines on the management of thyroid tumors by the Japan Associations of Endocrine Surgeons: Core questions and recommendations for treatments of thyroid cancer. Endocr J. Published online 2020:669-717. doi:10.1507/endocrj.ej20-0025